Monique Middlekauff |
April
12, 2019

How Do We Acknowledge Pelvic Floor Dysfunction and Provide Sound Training Advice for Female Athletes and Clients?
Key Points:
1. Pelvic floor disorders are not discussed, yet impact 25% of all women.
2. Identifying and addressing training concerns will help to improve client retention and better meet the needs of clients and athletes.
3. Simple and helpful talking points can give you the language to have conversations about pelvic floor health.
Many personal trainers and coaches have extensive knowledge of anatomy, applied physiology, and strength and conditioning principles. While much is understood and applied appropriately to female athletes and clients, there has been a large gap in the conversations and education provided to the exercise science community regarding the function of the pelvic floor and its role in performance.
Frankly, the topic of the pelvic floor often makes people feel uncomfortable. It is often skipped in academic courses, avoided in strength and conditioning material, and excluded from education material required for certifications. Due to lack of understanding, the pelvic floor is mistakenly thought to play an insignificant role in performance and health.
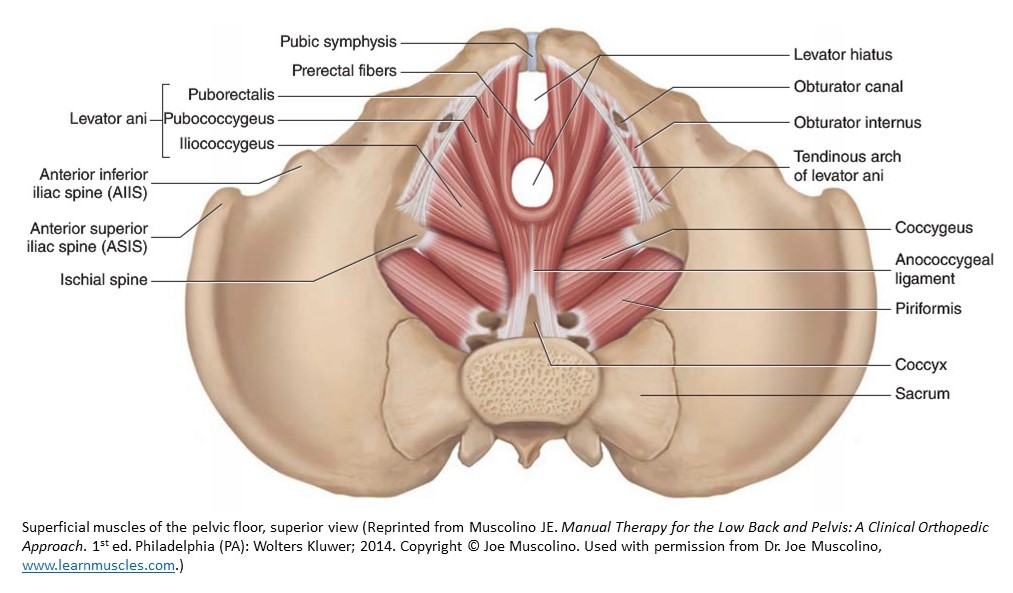
For purposes of clarification, the pelvic floor is a set of muscles, ligaments and connective tissue in the lowest part of the pelvis that provides support for the internal organs, including the bowel, bladder, uterus, vagina and rectum. Both men and women have a pelvic floor, yet more women experience dysfunction. Just as we wouldn't expect our biceps to get stronger by doing more squats, the same is true with the pelvic floor. If we don't specifically work on the pelvic floor muscles, they won't magically improve.
With intentional consideration, trainers and coaches can help women at any level
of performance increase her physical fitness and reduce risk of pelvic floor damage.
A quarter of all women (1 in 4) will experience a pelvic floor disorder in their lifetime. The pelvic floor serves a major role in movement due to the function it serves in posture, balance, stability and strength. Dysfunction can cause back pain, balance and stability concerns and decreased athletic performance, especially noted during exercise that produces high intra-abdominal pressure like gymnastics, volleyball, jumping and high intensity weight lifting.
As more women are participating in high impact activity, it is important for coaches, trainers and physiologists to understand the potential harm (and benefits) of exercise programming on the pelvic floor.
What is a Pelvic Floor Disorder?
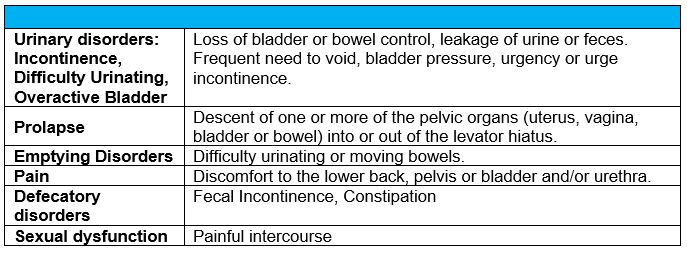
A grouping of disorders affecting the anatomy and functionality of the pelvic floor. A pelvic floor disorder often occurs when there is weakened pelvic floor muscles or tears in the connective tissue which may be due to excessive strain on the pelvis. There are many types of pelvic floor disorders, but many can be grouped into the following categories as seen in Table 1.1.
Table 1.1: Types of Pelvic Floor Disorders
Coaches, trainers and physiologists need to be aware of the potential pelvic floor problems that their athletes may be dealing with, and responsibly inform athletes about pelvic floor health. Leaking urine with exercise may be common, but it should not go untreated. Depending on the sport, women have been shown to have 26 to 67 percent of leakage during sport participation. We incorrectly assume that strong women have a strong pelvic floor. This simply isn’t the case, and this assumption can cause us to ignore a simple fix: specific exercise. We know the principle of specificity yet fail to apply it to all skeletal muscle. If the addition of active pelvic floor exercises does not help or even exacerbates the symptoms, it may be because the individual already has a tight shortened pelvic floor. This client may require a medical assessment and/or specialized pelvic floor physical therapy.
Participation in impact sport has an associated risk, but many female athletes have never been informed of the training practices that can reduce the risk for pelvic floor dysfunction. As an athlete, this was never discussed with me in any capacity. I never had a coach or trainer discuss ways to reduce my risk or ways to prevent issues later in life. As a researcher and educator, I was upset that this simple knowledge could help so many yet was not being discussed in the areas that help clients and athletes most.
High intensity exercise should be encouraged for those who are prepared for it. Significant attention is paid to lower extremity landing mechanics during jumping. Little-to-no attention is paid to breathing mechanics during landing to reduce the intra-abdominal pressure, pressing down on the pelvic floor, and potentially reducing support.
A healthy pelvic floor should expand and contract. Pelvic floor weakness and lack of support can be problematic. A pelvic floor that cannot relax also can be problematic. Just as with other muscles, we need strength and flexibility. Many people improperly tell women to just “do more Kegel exercises” without context of sets, repetitions or duration of exercise. Most women don’t know how to contract their pelvic floor muscles and most co-contract the abdominal muscles.
New client retention is a concern for personal trainers. Ask a question about pelvic symptoms or incontinence on intake. If you have a new client with a pelvic floor disorder, acknowledge their potential concerns and provide a welcoming and thoughtful solution. Women over 50, those with multiple deliveries, previous or current smokers, victims of sexual assault or those who regularly do high impact exercise are at additional risk for a pelvic floor disorder.
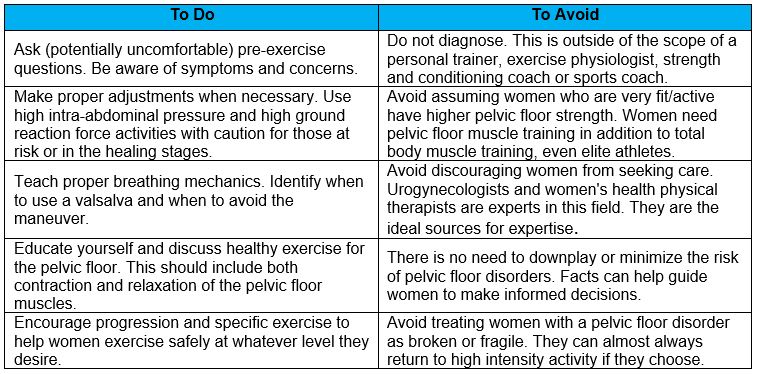
Higher intensity exercise is often programmed for women who are looking to lose body fat (e.g., Burpees, jumping jacks, sprints, box jumps, double-unders, squat jumps, etc.). Women with a pelvic floor disorder may self-select out of these activities without communicating why. Be considerate and provide helpful guidance and information to safely exercise with and without a pelvic floor disorder. The scope of a coach, personal trainer or clinical exercise physiologists should never be to diagnose pelvic floor dysfunction, but it is within their scope to direct exercise safely and find an exercise load that is safe and appropriate. Table 1.2 is a simple list of the ideal things to do and avoid for personal trainers and coaches regarding pelvic floor function.
Table 1.2: To Do and To Avoid for the Personal Trainer and Coach
Helpful talking points to teach new clients or athletes:
- “The pelvic floor muscles need exercise, just like any other muscle. Learn how to contract and fully relax your pelvic floor. This will be very helpful in keeping your pelvic floor muscles healthy while you exercise at higher loads.”
- “Chronic straining and constipation increases your chance of developing pelvic organ prolapse. Choose a high fiber diet and hydrate sufficiently. A diet with plenty of fiber and fluids helps to maintain regular bowel function. Persistent constipation increases risk for pelvic organ prolapse.”
- “While it may not be important for your sport or exercise, it is important for your health to reach and maintain a healthy body weight. This is even more important if you are going to do high impact activity. Additional abdominal weight may weaken the pelvic floor with high intra-abdominal pressure. Overweight women are at a significantly increased risk of developing prolapse.”
- “If you smoke, find support to quit. Smoking increases your risk of pelvic floor dysfunction.”
- “Use proper body mechanics when lifting, especially heavy loads.”
- “Regular physical activity helps maintain normal weight, as well as regular good bowel function. Pelvic floor muscle exercises (known as Kegels) improve the strength of the pelvic floor and limit the likelihood of developing stress incontinence and prolapse.”
- “Chronic cough increases abdominal and pelvic pressure and should be treated.”
With intentional consideration, trainers and coaches can help women at any level of performance increase her physical fitness and reduce risk of pelvic floor dysfunction. A potentially uncomfortable conversation can reduce barriers to physical activity. It also can provide profoundly needed education while building trust and connection.
Author: 
Monique Middlekauff has a PhD in Exercise Physiology from the University of Utah. She is an ACSM Clinical Exercise Physiologist (ACSM-CEP). Monique is certified in Advanced Cardiac Life Support through the AHA and is recognized as a Higher Education Teaching Specialist (HETS). As a former NCAA DI athlete, she enjoys high intensity training and experimenting with new exercise science techniques. Monique manages a Lifestyle Medicine clinic where she lives in Idaho. She enjoys boating and exploring outdoors.