In June of 2016 the United States Department of Health and Human Services convened the 2018 Physical Activity Guidelines Advisory Committee (PAGAC) under the Federal Advisory Committee Act of 1972. The charge given to the 2018 PAGAC was to independently review, appraise and summarize the current evidence linking physical activity to human health and function adhering to the best practices of systematic reviews, and deliver this information in a Scientific Report (6) that served as the foundation for the policy document, Physical Activity Guidelines for Americans, 2nd edition (7), released in November of 2018. Hypertension was chosen as a health condition to address in the 2018 PAGAC Scientific Report due to its importance as a public health problem, and the voluminous expansion of the literature on the topic of exercise and hypertension since the 2008 PAGAC Report (8). The ACSM new Pronouncement on exercise and hypertension contains the seminal portions of sections in the 2018 PAGAC Scientific Report on the use of exercise to prevent and treat hypertension (9). This blog highlights what’s new in the Pronouncement about exercise and hypertension (9), presents other new, relevant information from the 2018 PAGAC Scientific Report on exercise prescription for hypertension (6) and concludes with the new ACSM Frequency, Intensity, Time, and Type or FITT recommendations for hypertension. Of note, the 2018 PAGAC adhered to the JNC 7 blood pressure (BP) classification scheme (2) in the Pronouncement (9) because the literature reviewed was based upon this BP classification scheme. As of Feb 2018, which was the end of our systematic literature search, there were no meta-analyses or systematic reviews published that did not utilize the JNC 7 blood pressure classification scheme. However, BP is a continuous variable and the law of initial values applies regardless of the cutoffs used (i.e., JNC 7 or ACC/AHA). As such, none of the key findings differ in any way regarding the FITT exercise prescription for hypertension.
These BP improvements occur: 1) immediately and persist up to 24 hours after a single exercise session, termed postexercise hypotension (4), an exercise session that can be of any duration performed continuously or accumulated to total > 20-30 minutes per day; 2) with as little as 90 min per week of exercise training; and 3) after aerobic or resistance exercise performed alone or combined, termed concurrent exercise. Please see the Figure adapted from Cornelissen and Smart (11), MacDonald et al. (12), and Corso et al. (13) that shows resistance exercise now measures up to aerobic exercise as antihypertensive lifestyle therapy. This new finding is a departure from previous exercise and hypertension guidelines that recommended aerobic over dynamic resistance exercise for the prevention and treatment of hypertension (3-5). The evidence for complementary and alternative types of exercise, such as Baduanjin, Qigong, Tai Chi, and Yoga, was promising but too limited to be emphasized alongside aerobic and resistance exercise at this time.
3. Among adults with hypertension, exercise lowers the risk of: 1) the progression of cardiovascular disease as evidenced by the BP reductions that result from exercise; and 2) cardiovascular disease mortality in dose-response fashion. Hu et al. (14) found adults that the risk of cardiovascular disease mortality was 25 percent lower among highly physically active adults than those that were physically inactive.
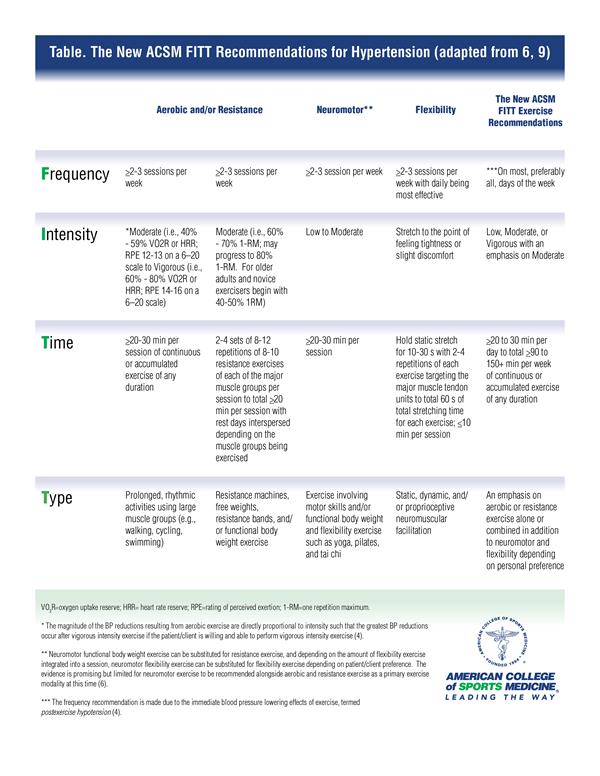
The New American College of Sports Medicine FITT Recommendations for Hypertension
Based upon the findings of the 2018 PAGAC Scientific Report (6) and
this ACSM Pronouncement (9), the new ACSM FITT recommendations for hypertension are revealed in the Table. Emphasis is no longer placed on aerobic exercise alone. Aerobic
or resistance exercise alone or aerobic and resistance exercise combined (i.e, concurrent exercise) are recommended on most, preferably all, days of the week to total 90 min to 150 min per week or more of multi-modal, moderate intensity exercise. The expansion of the ACSM FITT recommendations to include multi-modal exercise offers variety and more attractive exercise options that may translate to better exercise adherence for adults with hypertension.
Download the FITT Recommendations.
Learn more about the Physical Activity Guidelines for Americans, 2nd Edition
Linda Pescatello, PhD, FACSM, is a Distinguished Professor of Kinesiology at the University of Connecticut. Her research on topics including exercise and hypertension, physical activity interventions and exercise genomics (among other topics) has been widely published. She was the recipient of an ACSM Citation Award in 2011, and served as the Senior Editor for ACSM's Guidelines for Exercise Prescription and Testing, 9th edition.
References
1. Whelton PK, Carey RM, Aronow WS, Casey DE,Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC,Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA S, Williamson JD, Wright JT,Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:1269–1324.
2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL,Jr, Jones DW, Materson BJ, Oparil S, Wright JT,Jr, Roccella EJ, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung,and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42(6):1206-52.
3. ACSM Guidelines for Exercise Testing and Prescription 10th Edition. Riebe, D (senior ed.) and Ehrman, JK, Liguori, G, and Magal, M (assoc. eds.). Philadelphia, PA: Wolters Kluwer Health, 2018.
4. Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA, American College of Sports Medicine. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004; 36(3):533-53.
5. Pescatello LS. Exercise measures up to medication as antihypertensive therapy: Its value has long been underestimated. Br J Sports Med 2018 Dec 19. pii: bjsports-2018-100359. doi: 10.1136/bjsports-2018-100359. [Epub ahead of print] PMID: 30567705.
6. Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report, 2018. Washington, DC: U.S. Department of Health and Human Services.
7. US Department of Health and Human Services. 2018 Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: US Department of Health and Human Services; 2018.
8. Physical Activity Guidelines Advisory Committee. 2008 Physical Activity Guidelines Advisory Committee Scientific Report, 2008. Washington, DC: U.S. Department of Health and Human Services.
9. Pescatello LS, B Bloodgood, D Buchner, W Campbell, S Dietz, L DiPietro, S George, JM Jakicic, WE Kraus, A McTiernan, RR Pate, K Piercy, KE Powell and RF Macko, for the 2018 Physical Activity Guidelines Advisory Committee. Physical activity to prevent and treat hypertension. On Behalf of the 2018 Physical Activity Guidelines Advisory Committee. Med Sci Sports Exerc (in press).
10. Liu X, Zhang D, Liu Y, et al. Dose-Response Association Between Physical Activity and Incident Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Hypertension. 2017; 69(5):813-820.
11. Cornelissen, VA, Smart, NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013b. 2(1):e004473
12. MacDonald, HV, Johnson, BT, Huedo-Medina, TB, et al. Dynamic Resistance Training as Stand-Alone Antihypertensive Lifestyle Therapy: A Meta-Analysis. J Am Heart Assoc. 2016. 5(10):#pages#
13. Corso, LM, Macdonald, HV, Johnson, BT, et al. Is Concurrent Training Efficacious Antihypertensive Therapy? A Meta-analysis. Med Sci Sports Exerc. 2016. 48(12):2398-2406
14. Hu G, Jousilahti P, Antikainen R, Tuomilehto J. Occupational, commuting, and leisure-time physical activity in relation to cardiovascular mortality among finnish subjects with hypertension. Am J Hypertens. 2007; 20(12):1242-50.