Diba Mani, Ph.D. |
Feb.
20, 2020
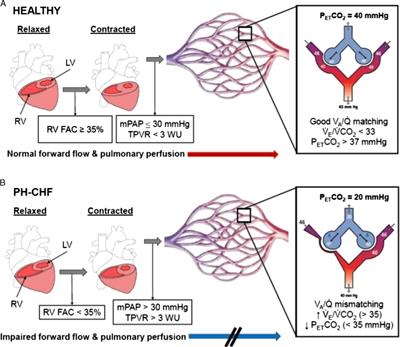 Worldwide, 17%-45% of patients admitted to a hospital for heart failure will die within the year. The range narrows for the U.S. (25%-35%) and Europe (17%-30%). Chronic heart failure is characterized by changes in multiple body systems, including the cardiac, vascular, musculoskeletal, endocrine and pulmonary. Not surprisingly, a patient’s capability to exercise is impacted by the severity of symptomology. Cardiac function, as measured by variables such as cardiac output and left ventricular volume, has interestingly not been shown to be associated with exercise tolerance in these patients. Rather, as the authors of a recent paper, “Exercise Intolerance in Heart Failure: Central Role for the Pulmonary System” published in Exercise and Sport Sciences Review—Sophie Lalande, Troy J. Cross, Manda L. Keller-Ross, Norman R. Morris, Bruce D. Johnson, and Bryan J. Taylor—expand on, the exercise intolerance exhibited by patients stems from various factors originating in various body systems with the most negatively affected being the pulmonary system. Lalande and colleagues elaborate on the role the pulmonary system plays in exercise limitation in patients with chronic heart failure.
Worldwide, 17%-45% of patients admitted to a hospital for heart failure will die within the year. The range narrows for the U.S. (25%-35%) and Europe (17%-30%). Chronic heart failure is characterized by changes in multiple body systems, including the cardiac, vascular, musculoskeletal, endocrine and pulmonary. Not surprisingly, a patient’s capability to exercise is impacted by the severity of symptomology. Cardiac function, as measured by variables such as cardiac output and left ventricular volume, has interestingly not been shown to be associated with exercise tolerance in these patients. Rather, as the authors of a recent paper, “Exercise Intolerance in Heart Failure: Central Role for the Pulmonary System” published in Exercise and Sport Sciences Review—Sophie Lalande, Troy J. Cross, Manda L. Keller-Ross, Norman R. Morris, Bruce D. Johnson, and Bryan J. Taylor—expand on, the exercise intolerance exhibited by patients stems from various factors originating in various body systems with the most negatively affected being the pulmonary system. Lalande and colleagues elaborate on the role the pulmonary system plays in exercise limitation in patients with chronic heart failure.
The paper does an excellent job of elaborating on the physiological impact of chronic heart failure on the pulmonary system, which includes modifications to airway blood flow, lung diffusing capacity and intrathoracic pressure. For example, engorgement of the bronchial vasculature may result in a narrowing of the internal diameter of compliant airways and contribute to increased airway resistance seen in patients. Alternatively, the capability of the lungs to diffuse carbon monoxide is significantly altered between healthy controls and patients with heart failure during both rest and exercise (as noted by Olson et al. in 2006 and 2016 articles), which indicates a lower pulmonary capillary blood volume and inability to transfer gases through the alveolar-capillary membrane.
Needless to say, skeletal muscle plays a role, too! In 1996, AJ Coats published a paper on the “muscle hypothesis” of chronic heart failure in The Journal of Molecular and Cellular Cardiology, which suggests that cardiac patients experience skeletal muscle myopathies, which contribute to issues such as skeletal muscle fatigability and exercise intolerance. Interventions to prevent or at least limit the muscle wasting and shift in fiber type distribution are vital, especially given repeated evidence validating the contribution of skeletal muscle to augmented ventilator response and exercise intolerance in patients with heart failure. The authors go on to elaborate on these adjustments and several others.
Treatment of pulmonary indications is clearly a first step in reintroducing physical activity into the lives of patients living with chronic heart failure. Of course, issues remain: how do we treat these pulmonary manifestations of heart failure when the typical course is to adopt an exercise training intervention? What sort of prescription guidelines can we share with clinicians to safely prescribe patients who have clear limitations in exercise tolerance?
How can you help your students better grasp the concepts of the central role of the pulmonary system on exercise intolerance in heart failure? Check out the online-only Journal Club questions by the authors to help students think critically about the topic, including:
What are some of the strategies that could lead to an improved exercise tolerance in heart failure?
 Diba Mani, Ph.D., is a lecturer in the Department of Applied Physiology & Kinesiology at the University of Florida. She serves as the Digital Editor for Exercise and Sport Sciences Reviews. She earned her degrees under the mentorship of Dr. Roger Enoka in the Neurophysiology of Movement Laboratory at the University of Colorado. Her doctoral dissertation focused on evaluating the effects of electrical nerve stimulation on motor unit discharge properties and mobility in young and older adults. Dr. Mani most enjoys the human component of any work she is engaging in, be it research in the field of geriatrics or teaching college students in the classroom. Dr. Mani is a nationally certified judo referee and coach and also a regular vinyasa yoga practitioner. She is passionate about diversity and cultural promotion through involvement in groups such as Iranian American Academics & Professionals and the Persian Students Organization.
Diba Mani, Ph.D., is a lecturer in the Department of Applied Physiology & Kinesiology at the University of Florida. She serves as the Digital Editor for Exercise and Sport Sciences Reviews. She earned her degrees under the mentorship of Dr. Roger Enoka in the Neurophysiology of Movement Laboratory at the University of Colorado. Her doctoral dissertation focused on evaluating the effects of electrical nerve stimulation on motor unit discharge properties and mobility in young and older adults. Dr. Mani most enjoys the human component of any work she is engaging in, be it research in the field of geriatrics or teaching college students in the classroom. Dr. Mani is a nationally certified judo referee and coach and also a regular vinyasa yoga practitioner. She is passionate about diversity and cultural promotion through involvement in groups such as Iranian American Academics & Professionals and the Persian Students Organization.