Lisa Hoffman, MA |
May
24, 2021

Practical Strategies to Implement Parkinson’s Exercise Guidelines
Parkinson’s and Exercise
To understand the role exercise plays in treating Parkinson’s disease (PD), we first need to understand the symptoms of the disease. Parkinson’s is a progressive, neurodegenerative disorder that affects about one million people in the United States and 10 million people worldwide. It is called a movement disorder because of the “motor features” it can cause – tremors, slow movements, stiffness and muscle cramping. Symptoms are diverse and usually develop slowly over time. Parkinson’s not only disrupts brain networks that control movement, but also those linked to mood, behavior and thinking (cognition).
The symptoms of Parkinson’s disease include more than just the motor features. Parkinson’s impacts thinking: the disease can affect working memory, decision-making, staying attentive and concentration. Parkinson’s is also linked to depression and anxiety, and it can affect behavior and disturb sleep.
Research from the Parkinson’s Foundation Parkinson’s Outcomes Project, the largest-ever clinical study of Parkinson’s, suggests that people with PD do at least 2.5 hours of exercise a week for a better quality of life. Exercise is increasingly accepted as an adjunct treatment for Parkinson’s disease.
The Role of Exercise Professionals
Exercise professionals provide leadership, expertise and programs to help people living with PD achieve their goals and manage their Parkinson’s symptoms. These professionals should be considered an integral part of the interprofessional care team for people with Parkinson’s.
As a leader in driving better health outcomes and quality of life for people with Parkinson’s, the Parkinson's Foundation has created Exercise Guidelines for people with Parkinson’s and is in the process of creating a competency framework for Exercise Professionals to ensure that people with Parkinson’s are receiving safe and effective programs and instruction.
Exercise professionals provide leadership, expertise and programs to help people living with PD achieve their goals and manage their Parkinson’s symptoms.
Parkinson’s Exercise Guidelines | Resources
Parkinson’s Exercise Guidelines for People with Parkinson’s: Professional Version (External Link)
Parkinson’s Exercise Guidelines Video (External Link)
Miriam Rafferty, PT, DPT, PhD
Parkinson’s Exercise Recommendations for People with Parkinson’s (Infographic)
The guidelines include recommended frequency, intensity, time, type, volume, and progression (FITT-VP) of exercises that are safe and effective for people with Parkinson’s across four domains: aerobic, strengthening, flexibility, and balance.
The exercise guideline table contains information synthesized in previous versions of ACSM’s Guidelines for Exercise Testing and Prescription1 and ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities2. One large addition is the inclusion of a fourth column to highlight the importance of balance and agility exercises, including multitasking. Also highlighted is the importance of cognitive and behavioral considerations given the nonmotor symptoms of PD.
It is recommended that people with PD 1) see a physical therapist specializing in Parkinson’s for full functional evaluation and recommendations and 2) exercise during “on” periods when taking medication.
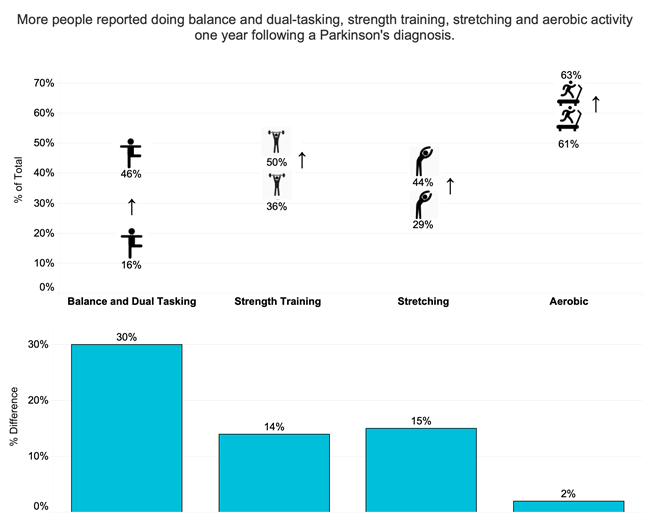
Figure 1: Change of Exercise Post Diagnosis: Balance, agility or dual-tasking was the type of exercise with the largest change before and a year after diagnosis, with an increase of 30.24%. Stretching and strength training also increased significantly.
Safety
Given the progressive nature of the disease and associated decline in physical function, there are some safety precautions and strategies to be aware of as exercises may need to be modified.
Orthostatic Hypotension: Orthostatic hypotension is a sudden drop in blood pressure when standing up from a seated or prone (lying down) position.
Risk of Falling: People living with PD are at a higher risk for falls due to the motor symptoms, including stiff muscles, freezing (temporary inability to move), and balance impairment.
Cognitive Challenges: Feelings of distraction, decreased executive function, or disorganization can accompany cognitive impairment, along with difficulty planning and accomplishing tasks.
Cueing Strategies: People with PD often depend on external cues during execution of motor tasks due to a loss of automaticity that may cause disruptions in processing intrinsic information.
Motivation to Move
Apathy, depression and fatigue are some of the non-motor symptoms of Parkinson’s that may hinder your client’s ability to participate in exercise. Although knowing the benefits of participating in physical activity, these and other non-motor symptoms are often overlooked and undertreated when motivating a client to exercise.
Exercise is an essential part of managing Parkinson’s disease and exercise professionals play a vital role in developing safe and effective programs to optimize quality of life for those living with PD.
Summary
1. People with Parkinson’s should find ways to participate in regular exercise targeting aerobic fitness, strengthening, flexibility, as well as balance, agility and multi-tasking.
2. Skilled and knowledgeable exercise professionals provide personal training and/or group exercise instruction for people with Parkinson’s, along with social support and motivation.
3. Exercise professionals may have more contact with people with PD than the traditional interprofessional healthcare team, providing great opportunity for positive impact on quality of life.
Learn More
The Parkinson’s Foundation believes in empowering the Parkinson’s community through education. Learn more about exercise and Parkinson’s at Parkinson.org/ExercisePros
Author:

Lisa Hoffman, MA is the Director of Professional Education at the Parkinson’s Foundation. She guided the inclusion of exercise professionals as part of the care team for people with Parkinson’s by initiating Development of Criteria for Exercise Education Programs & Competency Framework for Exercise Professionals. Lisa was the founder and director of Solo Fitness and Wellness, Inc. a NYC based in-home personal training company for 30 years. She earned her master’s degree from Columbia University in Applied Physiology, received her bachelor’s degree in Modern Dance from SUNY Brockport.
References
1. American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 10th ed. Baltimore (MD): Wolters Kluwer; 2017.
2. American College of Sports Medicine. ACSM's Exercise Management for Persons with Chronic Diseases and Disabilities. Champaign (IL): Human Kinetics; 2016.
DOWNLOAD your sample of ACSM's Guidelines book