by
Greg Margason
| Oct 26, 2023
Miss the webinar? Access it below.
Webinar Recording

 Q: In the carb loading studies, what method did they use to measure the glycogen stores?
Q: In the carb loading studies, what method did they use to measure the glycogen stores?
In the two studies described in the presentation muscle biopsies were used to measure muscle glycogen stores. The references for the two studies are listed below, if more information is required:
Tarnopolsky LJ, MacDougall JD, Atkinson SA, Tarnopolsky MA, Sutton JR. Gender differences in substrate for endurance exercise. J Appl Physiol. 1990 Jan;68(1):302-8. doi: 10.1152/jappl.1990.68.1.302. PMID: 2179207.
Tarnopolsky MA, Zawada C, Richmond LB, Carter S, Shearer J, Graham T, Phillips SM. Gender differences in carbohydrate loading are related to energy intake. J Appl Physiol. 2001 Jul;91(1):225-30. doi: 10.1152/jappl.2001.91.1.225. PMID: 11408434.
Q: What about ketogenic diets and its impact on female athletes (performance/body composition etc.).
Burke et al (2020) investigated the effects of high fat low carbohydrate diets on female race walkers and found impaired exercise economy and performance. This data suggests that a high fat diet is not conducive for endurance performance. Endurance athletes should undertake a cost/ risk analysis of consuming a high fat/ low carbohydrate diet and understand the potential impairments that it might have on higher intensity exercise.
Burke LM. Ketogenic low-CHO, high-fat diet: the future of elite endurance sport? J Physiol. 2021 Feb;599(3):819-843. doi: 10.1113/JP278928. Epub 2020 Jun 10. PMID: 32358802; PMCID: PMC7891323.
Q: Could the male athletes oxidize [carbohydrate] more because they have more available to be used (if females tend to be under supplied)?
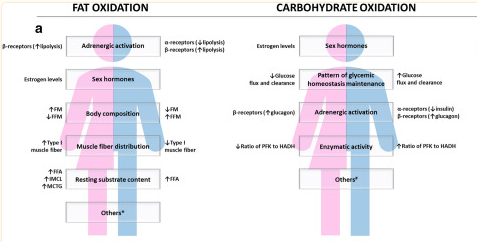
Women use more fat and less carbohydrate compared to men during endurance exercise. This is likely due to the higher levels of the female sex hormone estrogen. Studies have found that when estrogen is administered to men higher fat oxidation rates are seen. Although estrogen might explain some of the sex differences in substrate metabolism the exact mechanisms are not fully known and are likely to be multifactorial. A meta-analysis by Cano et al gathered mechanistic insights into the possible reasons for the sex-based differences in substrate utilization and produced the thematic diagram.
Cano A, Ventura L, Martinez G, Cugusi L, Caria M, Deriu F, Manca A. Analysis of sex-based differences in energy substrate utilization during moderate-intensity aerobic exercise. Eur J Appl Physiol. 2022 Jan;122(1):29-70. doi: 10.1007/s00421-021-04802-5. Epub 2021 Sep 22. Erratum in: Eur J Appl Physiol. 2022 Jul;122(7):1749. PMID: 34550468; PMCID: PMC8748379.
Q: It appears most of the studies have investigated endurance training and aerobic sports. What (if anything) does the literature indicate about carbohydrate consumption and usage during resistance training in women with the goal of building muscle mass?
There are some studies that have investigated energy metabolism during anaerobic sprint type exercise. A review by Boisseau & Isacco (2022) conclude that glucose regulation is not different between men and women during short bouts of high intensity exercise. Regarding carbohydrate intake the current carbohydrate recommendations are currently not sex specific and are based on exercise duration. Regardless of exercise type the recommendations state that when training for longer than 60 minutes, the recommended amount of carbohydrate is 30-60 g/h.
Nathalie Boisseau & Laurie Isacco (2022) Substrate metabolism during exercise: Sexual dimorphism and women’s specificities, European Journal of Sport Science, 22:5, 672-683, DOI: 10.1080/17461391.2021.1943713
Q: Is there research you can suggest that has investigated post-menopausal female athletes? Q: Be good to get an opinion on nutritional support for peri- & menopausal athletes and if there is a recommended substrate manipulation in those populations? Q: what are the implications for female athletes post menopause?
Menopausal women may have lower rates of fat oxidation at rest and during exercise compared to pre-menopausal women. This might be explained by the reduction in estrogen levels as well as the decrease in lean mass during menopause. There are currently no specific sports nutrition recommendations for post-menopausal women however in a review by Smith-Ryan et al (2022) it states that 24-h energy expenditure decreases with age, as well as a decrease in skeletal muscle balance and a blunted anabolic response to protein ingestion. These things should be taken into consideration when implementing any dietary recommendations for menopausal women.
Here is a reference for further reading, although this study was not performed in female athletes: Abildgaard J, Pedersen AT, Green CJ, Harder-Lauridsen NM, Solomon TP, Thomsen C, Juul A, Pedersen M, Pedersen JT, Mortensen OH, Pilegaard H, Pedersen BK, Lindegaard B. Menopause is associated with decreased whole body fat oxidation during exercise. Am J Physiol Endocrinol Metab. 2013 Jun 1;304(11):E1227-36. doi: 10.1152/ajpendo.00492.2012. Epub 2013 Apr 2. PMID: 23548615.
Smith-Ryan AE, Cabre HE, Moore SR. Active Women Across the Lifespan: Nutritional Ingredients to Support Health and Wellness. Sports Med. 2022 Dec;52(Suppl 1):101-117. doi: 10.1007/s40279-022-01755-3. Epub 2022 Sep 29. PMID: 36173598; PMCID: PMC9521557.
Q: Was body composition recorded when measuring fat v cho use during exercise? i.e... did women have higher body fat and is that why men relied more on cho when exercising in a fasted state. Q: when comparing male and female substrate utilization during fasting endurance exercise were the results adjusted for percentage body fat?
Women have been found to have greater intramuscular triglycerides concentrations than men, this difference could explain the higher rates of fat oxidation as these lipids stores in the muscle are a significant energy source. In fact, a study by Randell et al (2016) found absolute maximal fat oxidation (MFO) rates to be higher in male athlete compared to females (0.61 and 0.50 g∙min-1 respectively, P < 0.001). However, when expressed relative to fat free mass (FFM), MFO were higher in the females compared to males (MFO/FFM: 11.0 and 10.0 mg∙kg∙FFM-1∙min-1 respectively, P <0.001).
Steffensen, C. H., Roepstorff, C., Madsen, M., & Kiens, B. (2002). Myocellular triacylglycerol breakdown in females but not in males during exercise. American Journal of Physiology- Endocrinology and Metabolism, 282(3), E634–E642. doi:10. 1152/ajpendo.00078.2001
Randell RK, Rollo I, Roberts TJ, Dalrymple KJ, Jeukendrup AE, Carter JM. Maximal Fat Oxidation Rates in an Athletic Population. Med Sci Sports Exerc. 2017 Jan;49(1):133-140. doi: 10.1249/MSS.0000000000001084. PMID: 27580144.
Q: Are there specific recommendations around how much time an athlete can be in a reduced energy availability state before concerns arise?
In the new IOC consensus statement introduces the term “adaptable low energy availability”. The definition is as follows:
“Adaptable LEA is exposure to a reduction in energy availability that is associated with benign effects, including mild and quickly reversible changes in biomarkers of various body systems that signal an adaptive partitioning of energy and the plasticity of human physiology. In some cases, the scenario that underpins the reduction in energy availability (eg, monitored and mindful manipulation of body composition or scheduled period of intensified training or competition) might be associated with acute health or performance benefits (eg, increased relative VO2max). Adaptable LEA is typically a short-term experience with minimal (or no) impact on long-term health, well-being or performance. Moderating factors may also alter the expression of outcomes.”
This paper also states that short-term low energy availability is defined as a few days to weeks, but this does require further investigation.
Mountjoy M, Ackerman KE, Bailey DM, et al British Journal of Sports Medicine 2023;57:1073-1097
Q: Did you say that there’s no research on how LEE affects female athletes?
There is an abundance of research that has been conducted on low energy availability in female athletes. The new IOC statement mentions that since 2018 there have been considerable scientific advancements in the Relative Energy Deficiency in Sport (REDs) research field including ~178 REDs and/ or LEA original research publications featuring ~23 822 participants; (80% female).
Mountjoy M, Ackerman KE, Bailey DM, et al British Journal of Sports Medicine 2023;57:1073-1097
Q: So, it appears that low energy availability is a problem with females and males. Is this why we see athletes that show no improvements in strength and performance?
Low energy availability is not evident in all athletes but can affect both male and female athletes. There are some potential REDs performance outcomes that might arise because of problematic low energy availability. Some of these performance outcomes do include decreased muscle strength and power performance. Research into this area has included both female and male athletes.
Mountjoy M, Ackerman KE, Bailey DM, et al British Journal of Sports Medicine 2023;57:1073-1097
Q: I work at a high-level tennis academy and with a number of high level teenage girls. I often encounter, when I ask what they have had for fuel, they either under fuel or eat nothing. I have started utilizing little snack bags with little things that they enjoy eating so that they can fuel for their practices etc. Any thoughts on this?
This is a great idea! This sounds like an easy and convenient way to increase energy intake.
Q: What are the top concerns practitioners should be aware of for female athletes in general when referring to carb loading?
I think practitioners need to be familiar with the science-based carbohydrate recommendations, but with their applied practitioner hat they need to deliver food and drink choices that are practical for the athletes to ingest. If an athlete (male or female) is about to compete in a match, competition, or race then carbohydrate ingestion acutely around the exercise occasion is important, but maybe on lower intensity or rest days the carbohydrate amounts can be reduced.
Q: What are your best recommendations on educating parents and coaches who discuss carbohydrates in a bad light and have influenced their athlete's ideas on carbohydrates? Q: for education on the importance of carb intake, what setting do you feel may be best for female athletes to learn about this information? Should it be from their coach, should an RD be required to meet individually with the athlete? Social media seems to be a great impact on the influence in intake.
As mentioned in my presentation education is key, how we best deliver the education is yet to be determined and I think this is largely because everyone consumes education in different ways. A lot of athletes use social media but social media posts are unregulated so there is a lot of misinformation. Finding credible sources on social media and directing athletes there would be one approach in helping to educate athletes. I believe that nutrition education should ultimately come from the RD, but I think there are opportunities to educate the whole multi-disciplinary team on certain nutrition topics so that everyone is speaking with the same voice.
Q: While using the -Q, let us say an athlete has scored >8. But it is the long-term injury sub-scale that has caused the score to be this high. The other two sub-scales of GI and Menses look fine. In that case, should we still consider the athlete to be Low on energy?
The IOC REDs Clinical Assessment Tool (CAT2) is recommended as a way to determine the severity of low energy availability in your athletes.
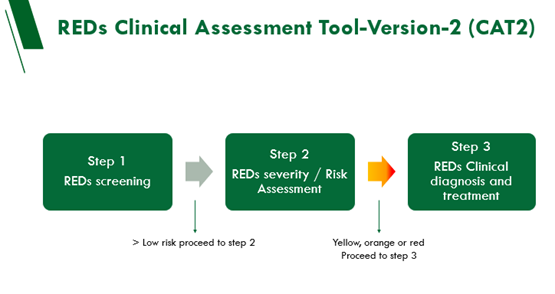
Mountjoy M, Ackerman KE, Bailey DM, et al British Journal of Sports Medicine 2023;57:1073-1097
Q: looking at iron levels in females, have you done research in showing the need to increase iron supplementation in female athletes?
Iron status and regulation in female athletes may be influenced by fluctuations in ovarian hormones and menstruation blood loss. Accordingly, the RDI for iron is 2.5 times higher in females, compared to males. There is a good article on the GSSI website on this topic:
https://www.gssiweb.org/en/sports-science-exchange/Article/micronutrient-considerations-for-the-female-athlete
Q: Would you mind listing the references you cited?
- Cowley et al., (2021) Sports Med. Women Sport Phys. Activity J. 29, 146–151
- Coyle et al. 1986, J Appl Physiol 61:165-172.
- Tarnopolsky, Atkinson, Phillips, & MacDougall,1995
- Tarnopolsky, Zawada, , Richmond, Carter, Shearer, Graham, & Phillips (2001).
- Hackney A.C. Horm. Metab. Res. 1990;22:647.
- Joint Positon Statement: Nutrition and Athletic Performance.Med Sci Sports Exerc. 48:543-68, 2016.
- Tanaka, Tanaka & Landis 1995, Int J Sport Nutr, 5:206-214.
- Moss SL et al (2021) Eur J Sport Sci. 21:861-870.
- Reed JL et al (2014) J Sport Sci. 32:1499-1509
- Martin L et al (2006) J Sport Sci Med. 5:130-137.
- McHaffrie SJ et al(2022). Sci Med Football. 6(5):675-685.
- Devries et al (2006) Am J Physiol Regul Integr Comp Physiol. Oct;291(4):R1120-8
- Cano et al Eur J Appl Physiol. 2022 Jan;122(1):29
- Wallis et al (2006) Am J Physiol Endo Meta. 290(4),E708–E715
- Derives et al (2006) Am J Physiol Regul Integr Comp Physiol. Oct;291(4):R1120-8;
- Hackney, A. C. (1999) ActaPhysiol Scandi,167(3),273–274.
- Zderic, T. W., Coggan, A. R., & Ruby, B. C. (2001). .J Appl Physiol,90(2), 447–453
- Heikura et al (2022) Eur J Sport Sci. 5:709-719.
- Ackerman et al (2019 Energy Deficiency in Sport. Br. J. Sports Med. 53:628-633
- Mountjoy M, Ackerman KE, Bailey DM, et al British Journal of Sports Medicine 2023;57:1073-1097