by
Caitlin Kinser
| May 13, 2022
 Two hot topics for athletes (and anyone interested in feeling/performing their best) right now are mental health and heart rate variability. For mental health awareness month, let’s talk about both!
Two hot topics for athletes (and anyone interested in feeling/performing their best) right now are mental health and heart rate variability. For mental health awareness month, let’s talk about both!
Mental performance and mental health exist on a continuum, and there’s frequent discussion in the world of sport psychology about distinctions, but one’s performance can impact their mental health and vice versa. An athlete may be so consumed with winning that impacts of performance anxiety bleed from hindered performance, and into general well-being. A soldier with PTSD might be unable to perform when it matters most. And a business executive may feel that they have to be “on” so frequently, that stress leads to obsessiveness, control issues, irritability and even depression. Examples of mental performance and mental health cross-over are limitless. By some estimates, one in five adults face mental health concerns in their lifetime and by other estimates, one in five adults face mental health concerns in a given year. In June of 2020 (during the pandemic), one estimate indicated that 40% of adults reported struggling with mental health or substance use, and by some recent accounts there is now a mental health crisis among teens. When mental health and/or performance suffers, heart rate variability (HRV) tends to be low; alternatively, higher HRV tends to be associated with reduced symptomology of depression or anxiety, improved cardiac functioning and better situational awareness.
People often say things like, “heart rate variability? Mine is pretty good, usually under 60 or 70.” However, they’re referring to heart rate (the number of times our heart beats in a minute). Heart rate variability (HRV) is a little bit different. With HRV, we are looking at how much the heart rate accelerates and decelerates, and whether or not fluctuations are rhythmic. While lower heart rate is often a good sign of cardiovascular functioning, higher HRV is a good indicator of both physical and psychological health. There are several ways to measure HRV; sport physiologists often use one metric to optimize training load (i.e., should I train hard today, go light or take a day off?). Psychophysiologists or performance psychologists may tap into other metrics to optimize stress management.
Through paced breathing and through stress management techniques, we can elevate heart rate variability. It’s like doing a workout to strengthen the vagal nerve, impacting nervous system functioning, to allow the sympathetic nervous system (“fight or flight”) to work in harmony with the parasympathetic nervous system (“rest and digest”). It also strengthens the baroreflex (responsible for blood pressure stabilization). In training HRV, the ups and downs in heart rate appear like a sine wave, whereby a rise in heart rate coincides with inhaling and decreases align with exhales; this is called respiratory sinus arrhythmia.
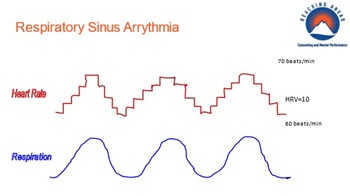 As you can see in the illustration, achieving respiratory sinus arrythmia (RSA) boosts HRV (the difference between max and min heart during rest or recovery). We can take this a step further, achieving RSA and maximizing the difference between peaks and valleys, by systematically determining one’s resonance frequency (RF). Simply put, this is the pace of breathing where HRV is maximized (according to max-min plus other HRV metrics). You can determine this with a biofeedback practitioner, and/or increasingly there are apps that will do this for you if you have a heart rate monitor. It can be worth it to go the distance to determine your exact RF rate, but most people tend to have an optimal breath rate in the ballpark of six breaths per minute, meaning: four second inhale and six second exhale. There are simple breath pacer apps that will help you pace your breath exactly, so you can utilize this science-based approach rather than jumping on the latest breathing fad. And if you want to take your breathing regimen to the next level, allow it to be mindful paced breathing.
As you can see in the illustration, achieving respiratory sinus arrythmia (RSA) boosts HRV (the difference between max and min heart during rest or recovery). We can take this a step further, achieving RSA and maximizing the difference between peaks and valleys, by systematically determining one’s resonance frequency (RF). Simply put, this is the pace of breathing where HRV is maximized (according to max-min plus other HRV metrics). You can determine this with a biofeedback practitioner, and/or increasingly there are apps that will do this for you if you have a heart rate monitor. It can be worth it to go the distance to determine your exact RF rate, but most people tend to have an optimal breath rate in the ballpark of six breaths per minute, meaning: four second inhale and six second exhale. There are simple breath pacer apps that will help you pace your breath exactly, so you can utilize this science-based approach rather than jumping on the latest breathing fad. And if you want to take your breathing regimen to the next level, allow it to be mindful paced breathing.
The next time you feel pulled to be supportive in response to another’s mental health or mental performance concerns by saying something like, “relax, take a deep breath,” consider the following tweak to your thinking/approach:
Mental health and mental performance concerns are common, especially now. Always err on the side of caution. Normalize struggles and validate feelings rather than jumping straight into “fix it mode.” Once they feel some empathy (or self-compassion, if it’s you!), allow your wording to incorporate HRV science. Say, “allow yourself to have a nice long exhale.” If the person you’re speaking with is intrigued, maybe suggest breathing with four second inhales and six second exhales, and perhaps even point them towards a breath pacer or a means of learning their more precise resonance frequency.
Access Mental Health Resources
 Tim Herzog, Ed.D., LCP, CMPC, BCB, is a licensed mental health provider in Maryland, Virginia, Pennsylvania, Rhode Island, Florida and Montana. He works with athletes nationally and internationally, and his practice, Reaching Ahead, is located in Annapolis, MD. Herzog is a Fellow with the Association for Applied Sport Psychology and serves on the organization’s Ethics Committee. He is a Certified Mental Performance Coach (CMPC), is listed on the USOPC Sport Psychology (2012 to present) and Mental Health (2021 to present) Registries and is Board Certified in Biofeedback (BCB). Mindful of the power of relationships, he conducts evidence-based practice, pulling from Cognitive-Behavioral Therapy, Acceptance and Mindfulness based approaches, Psychodynamic Psychotherapy and Interpersonal Process. Herzog also pulls wisdom from his years of coaching, notably having served as Head Coach of the Boston College Sailing Team 2001-2002, when the team placed 5th at ICSA Co-Ed Nationals and received 4 All-American honors (more than ever prior in BC history).
Tim Herzog, Ed.D., LCP, CMPC, BCB, is a licensed mental health provider in Maryland, Virginia, Pennsylvania, Rhode Island, Florida and Montana. He works with athletes nationally and internationally, and his practice, Reaching Ahead, is located in Annapolis, MD. Herzog is a Fellow with the Association for Applied Sport Psychology and serves on the organization’s Ethics Committee. He is a Certified Mental Performance Coach (CMPC), is listed on the USOPC Sport Psychology (2012 to present) and Mental Health (2021 to present) Registries and is Board Certified in Biofeedback (BCB). Mindful of the power of relationships, he conducts evidence-based practice, pulling from Cognitive-Behavioral Therapy, Acceptance and Mindfulness based approaches, Psychodynamic Psychotherapy and Interpersonal Process. Herzog also pulls wisdom from his years of coaching, notably having served as Head Coach of the Boston College Sailing Team 2001-2002, when the team placed 5th at ICSA Co-Ed Nationals and received 4 All-American honors (more than ever prior in BC history).